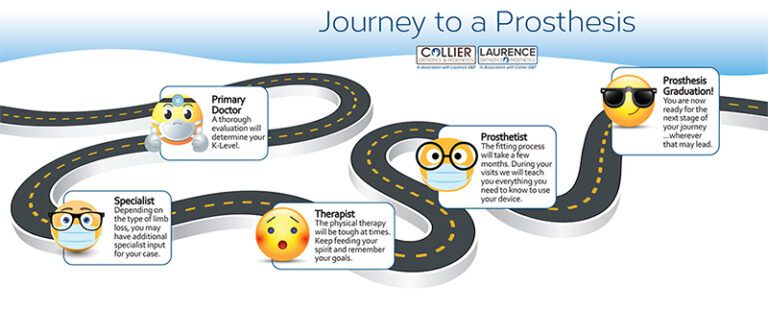
Helping those with limb loss find a prosthetist
Amputees and those with congenital disorders who wear a prosthetic device typically have a long-term relationship with their prosthetist. If you have never worn a prosthesis, this is an outline of what you should expect during your journey. Are you ready for a prosthesis? Obtaining a prosthesis is usually a long term process. You need…